
Recently, our doctors have told us that they are seeing more patients with complains about muscle pain or joint aches.
As we spend long hours sitting while working from home, combined with a lack of exercise, it could lead to an increase in weight due to more sedentary habits.
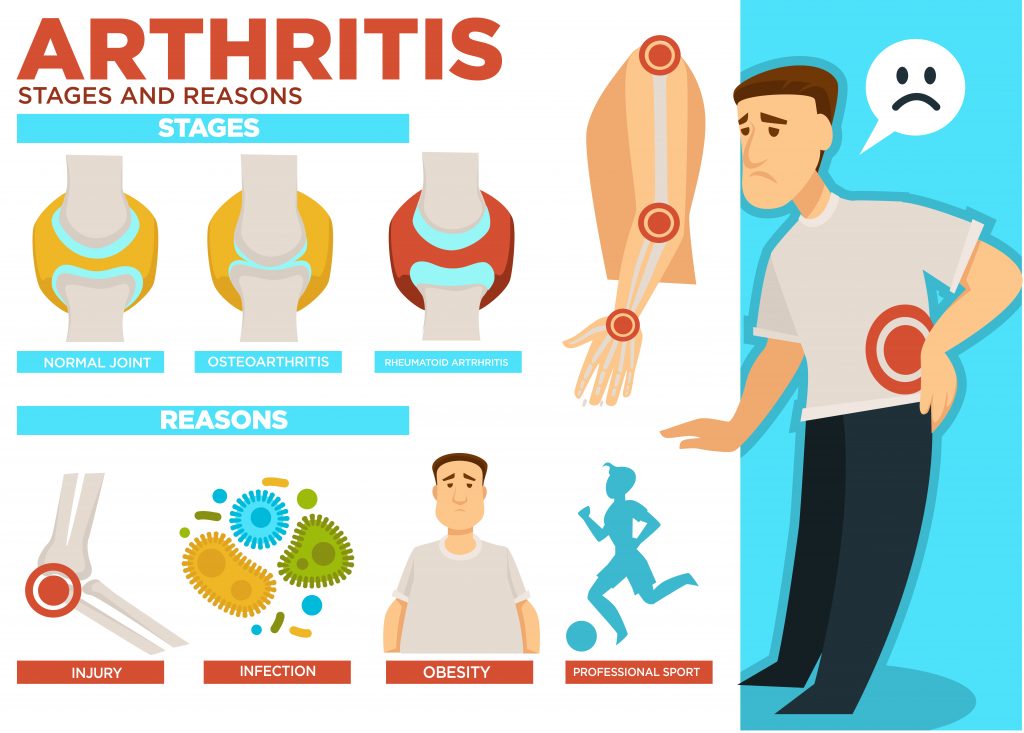
Osteoarthritis (OA) issues are also part of these numbers. Arthritis is a condition that causes joint pain. Did you know that diet plays a role in managing OA symptoms?
What is OA?
Osteoarthritis is the most common form of arthritis and is characterised by the wear and tear of the cartilage. It typically affects joints in the knees, hips, hands, the base of big toe and spine. Mainly made from water, cartilage protects and connects bones, nerves. In the joint, cartilage works as a cushion and shock absorber.
Why does it happen?
It can happen with a combination of factors such as obesity, age, injury, family history and muscle weakness.
Can diet help me?
The quality of your diet will have an impact on the pain and discomfort caused by OA.
Weight

Excessive body weight causes a strain in the joints. Excessive fat, especially around the waist increases inflammation that can increase the pain.
If you have a BMI higher than 23kg/m2 (if you are Asian) or 25/m2 (if you are non-Asian), losing only 10% of your body weight will not only result in relieving of OA symptoms but also improve your overall health. People with higher BMI and OA are at higher risk of having type 2 diabetes and cardiovascular disease, losing 10% of body weight will help prevent or manage these risks.
How to do this?
Some people express that it is difficult to lose weight because OA stops them from exercising. Following a healthy diet, with whole grains, fruits, and vegetables can do the trick. Check Health Promotion Board MyHealthy Plate for more information on how to follow a healthy and balanced diet.

Write a food diary
Keep a food diary; include quantities, cooking methods of everything you eat and drink. You should record your meals and drinks, immediately after you have them. At the end of the week, analyse it. Reflect the meals/food that you ate and how you can improve your diet the following week.
Exercise

Check with your doctor which exercises are safe for you to do. Swimming is a fairly safe exercise for most people as the water will support most of the body weight and reduce the tension over the joints. Start slow, increase the time and intensity of the exercise gradually. Most importantly be consistent and exercise regularly.
Seek help for a specialist to achieve a healthy weight loss
It is never easy to lose weight and to figure out which strategies are better to implement. You can also get some support from a dietitian.
Choose the right fats

Omega-3 fatty acids
Omega 3 found in oily fish and seaweed has anti-inflammatory properties that can improve your symptoms. Aim to have two portions of oily fish a week. Examples of oily fish are sardines, mackerel, salmon, herring and fresh tuna. You can also take fish oil capsules at a dose of around 450mg EPA+DHA per day. This dosage of fish oil may help reduce pain and improve muscles and joints function. It is also the recommended dose to reduce the risk of dying from cardiovascular disease.
Olive, canola and peanut oil
Choose monounsaturated fats over omega-6 polyunsaturated fatty acid and saturated fat.
Pick olive, canola and peanut oil over other types of oils. Omega 6 fatty acids and saturated fat are pro-inflammatory and may worsen your symptoms. If you often eat outside, opt for soup items and avoid oily and deep-fried foods. Usually, the type of oils used are either rich in saturated fats (e.g. palm oil or coconut) or polyunsaturated fats (e.g. sunflower oil, corn, safflower and grapeseed).
| Saturated fat | Mono-unsaturated fat | Omega-3 | Omega-6 | Trans fat |
| Red meat Full cream dairy products (ghee, butter, cream, cheese, full cream milk and yoghurt) Coconut oil Palm oil | Olive oil Canola oil Peanut Oil Olives, Avocado Almonds, Hazelnuts Peanuts | Oily fish Flax-seed, Canola oils Omega-3 eggs Walnuts, chia seeds | Chicken, turkey Sunflower oil Safflower oil Corn oil Grapeseed oil | Biscuits, cakes Chips Hard margarine Crackers (check labels) |
| Limit | Prefer | Prefer | Moderate | Avoid |
Improve your blood cholesterol
People with OA are more likely to have high cholesterol than those without. Reducing blood cholesterol will not only reduce your cardiovascular disease risk, but it may improve your symptoms.
Find out more about cholesterol here.
Here are some of the strategies that you can follow to reduce your blood cholesterol:
- Lose 10% of your body weight if you have a high BMI.
- Reduce intake of foods rich in saturated and trans fats.
- Increase the fibre on your diet with oats, barley, beans, peas, lentils and chickpeas
- Have nuts in your diet
- Consume soy products
Vitamins and antioxidants
Vitamin D
Vitamin D plays a vital role in bone and cartilage health. Studies show that vitamin D may help with muscular strength and balance. In Singapore, up to 42% of people have vitamin D deficiency.
Ask your doctor to check your vitamin D levels and discuss the best ways for you to increase your vitamin D status. The best way for our body to have vitamin D is through sunlight, but some people might benefit from supplementation.
Fruits, vegetables and whole grains
These foods are rich in vitamins, minerals, and antioxidants that may protect your joints and keep them healthier. Ensure that you eat a variety (and colours!) of vegetables and fruits, as well as including whole grains in your diet.
What about supplements?

There are plenty of supplements in the market, claiming that they can help with OA. A word of caution about supplements – they are not as strictly regulated as drugs are. Health supplements are not subjected to approvals and licensing by the Health Sciences Authority (HSA). For them to be accepted to enter the market, they do not need to prove that they work, just that its ingredients are safe and fall within HSA safety and quality standards.
While drugs must undergo rigorous clinical trials before entering the market, the same does not happen with supplements. As a result, studies that analyse the efficacy of supplements are scarce and often not very rigorous. Furthermore, when trials are conducted, usually only the studies that show benefits are published.
Here is a list of supplements that have shown some benefits, although more and more quality studies are needed to confirm efficacy. Most of these supplements seem to be safe. If you choose to take the supplements and you do not notice any changes in your pain and function after 4 to 6 weeks, then you should stop them.
- Curcumin
- Pine bark extract
- MSM (methylsulfonylmethane)
- Collagen hydrolysate
- Glucosamine (not for those with an allergy to shellfish)
- Chondroitin (not for those with an allergy to shellfish)
The bottom line
- Losing weight is your first and best strategy to manage OA as it will not only reduce the strain over your joints (especially your knees) but also reduce inflammation, reduce blood cholesterol and your cardiovascular disease risk.
- Follow a healthy diet that includes healthy monounsaturated oils and fatty fish (or fish oil), plenty of fruits and vegetables.
- Ask your doctor to check for your vitamin D status.
- Supplements are not reliable as they lack in quality research. If you are taking any supplement and you do not notice any difference after a few weeks, stop them.
- Make an appointment with a dietitian for guidance on how to improve your diet.
